BLOG

The Power of Patient-Centered Care for Hospice Patients
Patient-centered care isn’t just an idea—it’s a way of providing healthcare that puts patients’ needs, values, and choices at the heart of every decision. For case managers, social workers, and nurses, especially those helping patients transition
to hospice, this approach can transform care experiences for everyone involved. By prioritizing respect, collaboration, and compassion, patient-centered care improves patient outcomes, ensures dignity, and enhances satisfaction for patients
and families during their most vulnerable moments. Let’s explore what patient-centered care is, how it benefits hospice patients, and practical ways healthcare providers can bring it to life.
What is Patient-Centered Care?
At its core, patient-centered care is about creating meaningful partnerships between patients, families, and healthcare providers. It considers the whole person—not just their medical needs—by addressing emotional, cultural, and social factors.
Here’s how leading organizations define it:
-
Institute of Medicine: Patient-centered care respects and responds to individual patient preferences, needs, and values, ensuring these guide all clinical decisions.
Institute for Healthcare Improvement: This approach integrates cultural traditions, personal values, family situations, and lifestyles, making patients active members of the care team.
Patient-centered care moves away from the traditional “provider knows best” mindset. Instead, it emphasizes shared decision-making and collaboration, giving patients a voice in their care.
Why Shift to Patient-Centered Care?
Historically, healthcare was provider-focused, with professionals making decisions based on clinical expertise, often without patient input. While effective in some cases, this approach can ignore what matters most to patients and their families.
For hospice care, patient-centered care ensures:
-
Decisions align with the patient’s values and priorities.
Families feel heard and supported.
Care is compassionate and personalized.
Research supports its benefits:
A 2019 study in the Journal of General Internal Medicine found patient-centered care reduced hospitalizations and improved satisfaction scores.
Another study showed case management focused on this approach cut hospital admissions by 38% and saved an average of $18,000 per patient.
Principles of Patient-Centered Care
Patient-centered care is built on eight core principles that address every aspect of the patient experience. Picker Institute’s Eight Principles provide a comprehensive framework:
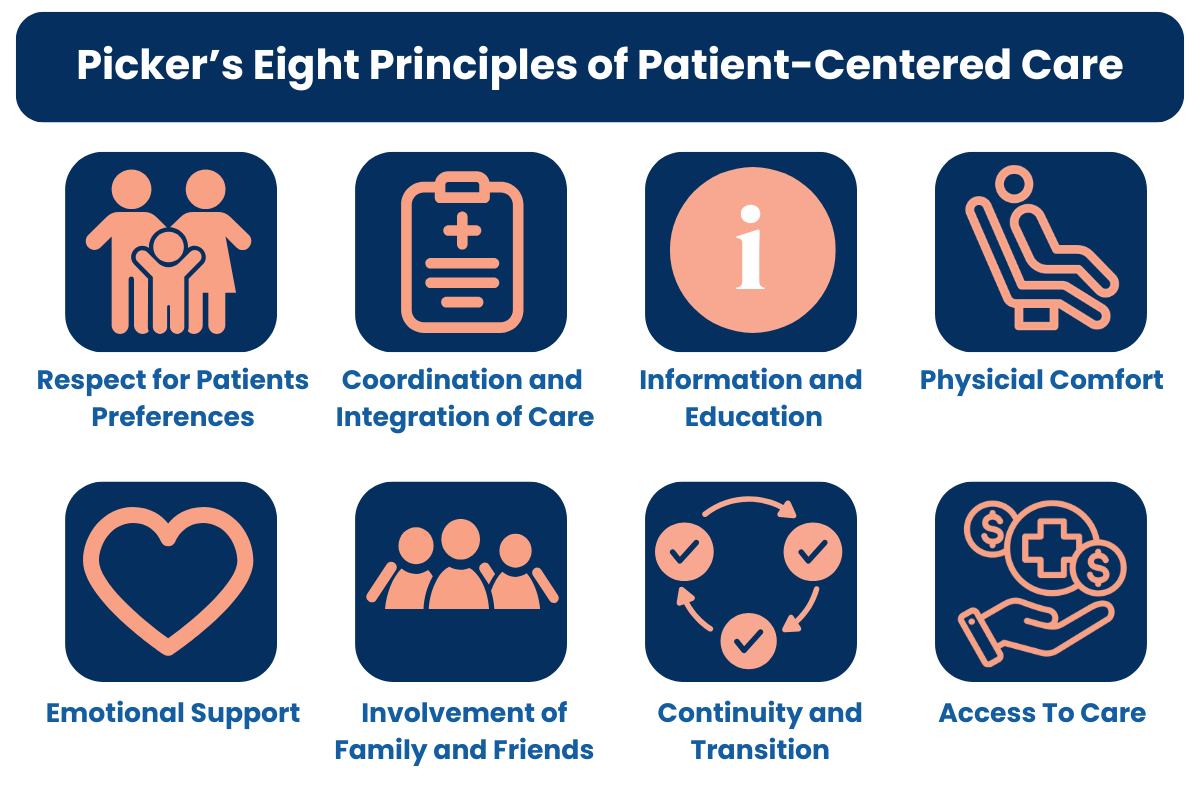
Respect for Patients’ Preferences: Honor patients’ values and needs by actively seeking their input on care plans.
Coordination and Integration of Care: Ensure smooth communication between teams to reduce stress for patients and families.
Information and Education: Offer timely and accurate information to empower patients to make informed decisions.
Physical Comfort: Manage pain effectively while attending to patients’ overall well-being.
Emotional Support: Address fears, anxiety, and the psychological impact of illness.
Involvement of Family and Friends: Include loved ones in decision-making and care.
Continuity and Transition: Provide seamless care transitions to avoid confusion.
Access to Care: Remove barriers to timely and necessary treatment.
For hospice care, these principles ensure patients and families feel supported throughout the journey, reinforcing dignity and trust.
Challenges in Patient-Centered Care
While rewarding, implementing patient-centered care isn’t always easy. Healthcare providers often face challenges such as:
Balancing Autonomy and Beneficence: Patients’ choices may differ from what healthcare providers believe is best. For example, a patient may prioritize staying alert over pain relief. These situations require respect and open conversations.
Time Constraints: Personalized care takes time, which can be limited in busy healthcare settings.
Organizational Resistance: Shifting to this model requires training and cultural change. A 2022 study in BMJ Quality & Safety found facilities with robust patient-centered care training saw a 25% improvement in outcomes and staff engagement.
Overcoming these challenges involves fostering a culture of respect, communication, and empathy.
Why It’s Essential for Seniors in Hospice
Elderly patients often have complex medical, emotional, and spiritual needs. Patient-centered care ensures they receive care that honors their values and goals.
Key Benefits for Hospice Patients:
Holistic Support: Care addresses emotional, spiritual, and psychological needs.
Personalized Pain Management: Pain relief plans respect each patient’s preferences.
Family Inclusion: Families are informed, involved, and supported throughout the journey.
Research shows this approach reduces anxiety and depression, improving quality of life in patients’ final months.
How to Know Patient-Centered Care is Working
You’ll know this approach is making a difference when:
Relationships Flourish: Patients and providers build trust and address each other by name.
Patients Feel Heard: They express their preferences and participate in decisions.
Outcomes Improve: Satisfaction increases, hospital readmissions decrease, and engagement grows.
These indicators reflect a positive shift toward compassionate, high-quality care.
Steps for Healthcare Professionals
Case managers, social workers, and nurses play vital roles in promoting patient-centered care. Practical steps include:
Encouraging Open Dialogue: Ask patients about their goals, fears, and preferences, and use this information to guide care.
Collaborating with Hospice Teams: Partner with providers like Unity Hospice and Palliative Care to design personalized care plans.
Educating Families: Provide resources and support to help families navigate the hospice experience.
Pursuing Continued Learning: Stay up to date on best practices through training and professional development.
By integrating these practices, healthcare professionals can create a supportive and respectful care environment.
Final Thoughts: A Compassionate Approach to Hospice
Patient-centered care transforms hospice experiences by putting patients’ needs, values, and preferences at the forefront of every decision. This approach not only improves outcomes but also fosters trust, dignity, and meaningful connections between patients, families, and healthcare providers.
By prioritizing respect, open communication, and collaboration, patient-centered care addresses the emotional, cultural, and spiritual dimensions of care, ensuring a holistic experience for patients and their loved ones. For healthcare professionals, adopting patient-centered care principles means embracing shared decision-making, personalized pain management, and family inclusion to enhance quality of life during the most vulnerable times.
It is a pathway to compassionate, high-quality care that aligns with patients’ goals and values, creating a more dignified and supportive hospice journey for all involved.
Discover More
At Unity Hospice and Palliative Care, we are here to support you in delivering personalized, dignified care. Together, we can make every moment meaningful for patients and families. Contact us today to learn how we can help you provide care and support for your patients who can benefit from hospice care.
Sources:
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. 2001.
- Institute for Healthcare Improvement. Patient-centered care: Examples and Best Practices. Accessed November 2024.
- BMJ Quality & Safety. “Impact of Patient-Centered Care Training on Staff and Patient Outcomes.” 2022.
- Journal of General Internal Medicine. “Benefits of Patient-Centered Case Management.” 2019.
- https://picker.org/who-we-are/the-picker-principles-of-person-centred-care/
