BLOG

Managing Heart Failure: The Role of Hospice & Palliative Care
Heart Disease: A Leading Cause of Death in the U.S.
Heart disease remains the leading cause of death in the United States, responsible for nearly 697,000 deaths annually—about 1 in every 5 deaths. Among cardiovascular conditions, heart failure is a major contributor to mortality and morbidity, affecting approximately 6.7 million Americans over age 20. Despite advancements in treatment, heart failure remains a progressive, incurable disease with significant symptom burden and frequent hospitalizations.
As healthcare professionals, we can improve patient outcomes by recognizing the role of palliative and hospice care in managing heart failure. These specialized services provide symptom relief, emotional support, and advanced care planning, ensuring patients receive the proper care at the right time.
Many heart failure patients struggle with symptom burden, financial constraints, and lack of understanding about their condition, which can lead to non-compliance with treatments. Additionally, these patients face an elevated risk of falls due to dizziness, fatigue, and fluid retention, which can further accelerate their decline and lead to hospitalizations.
Understanding Heart Failure and Its Impact
Heart failure is a lifelong condition in which the heart muscle cannot pump enough blood to meet the body’s needs. Patients experience a gradual decline in function, with symptoms such as:
Exercise intolerance
Unintentional weight loss
Fluid overload
Weakness
Anxiety and depression
Shortness of breath
Dizziness
Arrhythmias
Low blood pressure
Many patients with heart failure face frequent hospitalizations and reduced quality of life, making early intervention through palliative care and hospice essential.
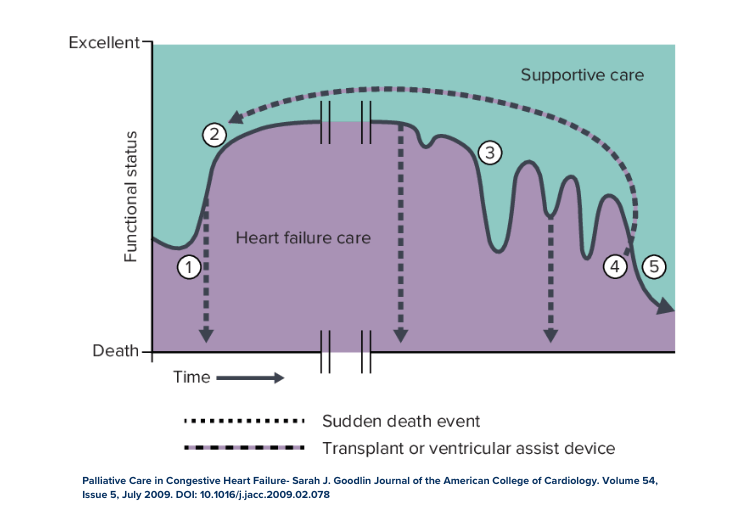
Heart failure follows a roller-coaster trajectory, where patients may temporarily improve with treatment but experience frequent exacerbations leading to hospitalizations.
This cycle places an immense emotional and financial burden on patients and their families. Studies show that 50% of people diagnosed with heart failure will not survive beyond five years, underscoring the need for proactive care planning.
The Role of Palliative Care in Heart Failure
Who Can You Refer to Palliative Care?
Palliative care is appropriate for patients with moderate to advanced heart failure who experience a significant symptom burden. We recommend referral for:
Patients requiring specialty care beyond primary cardiology who can benefit from enhanced symptom control and improved quality of life.
Patients with end-stage disease who wish to continue life-sustaining treatments can receive additional support to meet their needs.
Patients experiencing frequent hospitalizations and struggling with symptom distress.
Patients who have had repeated hospitalizations, significant weight loss, or are unable to tolerate standard heart failure treatments.
Patients and families who need guidance on goals of care and future treatment decisions.
Palliative care is especially valuable in bridging the gap between cardiology-focused disease management and holistic patient-centered care. Many cardiologists are focused on prolonging life but may not always address quality-of-life concerns, emotional distress, or future care planning. Palliative care teams help by offering a comprehensive approach that integrates symptom management, psychosocial support, and advanced care discussions.
Key Benefits of Palliative Care
Palliative care provides comprehensive support, including:
Symptom management (e.g., dyspnea, fatigue, fluid retention)
Psychosocial support for both patients and families
Disease education to help patients navigate treatment options
Prevention of hospitalizations by addressing needs in a home or outpatient setting
Goals of care discussions to align treatment with patient preferences
A study published in the Journal of the American College of Cardiology found that patients receiving ongoing, interdisciplinary palliative care showed significant improvements in quality of life, anxiety, depression, and spiritual well-being compared to those not receiving these services.
Since many patients and families lack a complete understanding of heart failure’s trajectory, palliative care also plays a critical role in educating them on treatment expectations, prognosis, and quality-of-life considerations. Early involvement in palliative care ensures patients make informed decisions before reaching a crisis point.
When to Transition to Hospice Care
Despite the benefits of palliative care, many heart failure patients transition to hospice too late, often within days of death. Early hospice referral allows patients and families to receive the full benefit of end-of-life support.
Hospice Eligibility Criteria for Heart Failure Patients
A patient may be eligible for hospice care if they meet the following criteria:
The patient is no longer a candidate for surgical intervention or declines further treatment.
The patient has New York Heart Association (NYHA) Class IV heart failure, characterized by severe limitations even at rest.
Supporting factors may include:
Treatment-resistant arrhythmias
History of cardiac arrest or resuscitation
Unexplained syncope
Brain embolism of cardiac origin
Concomitant HIV disease
In addition to these criteria, a rapid decline or multiple comorbidities may also indicate hospice eligibility.
Many heart failure patients can continue essential medications like diuretics while in hospice, ensuring comfort and quality of life. This is a common misconception among healthcare providers who believe that hospice requires stopping all medications. Instead, hospice focuses on maximizing comfort and minimizing distress, allowing patients to receive individualized care.
Hospice provides 24/7 access to care, reducing emergency hospital visits and helping families manage symptoms at home. Research also indicates that hospice can extend life expectancy by reducing unnecessary hospitalizations and improving symptom control.
Act Early to Help Ensure Patients Receive the Care They Deserve
Heart failure is a high-mortality, high-cost condition with a significant symptom burden. As healthcare professionals, we play a crucial role in ensuring that patients receive timely access to palliative care and hospice services.
How You Can Help:
Educate patients and families about their options early.
Identify patients who qualify for palliative or hospice care and refer them without delay.
Collaborate with palliative care teams to optimize symptom management and quality of life.
Encourage cardiologists to initiate early palliative care discussions to ensure patients receive comprehensive support.
By integrating palliative care and hospice into heart failure treatment plans, we can ensure that patients receive compassionate, patient-centered care throughout their journey.
Consider Unity for Your Heart Failure Patients
At Unity Hospice and Palliative Care, we support you in delivering personalized, dignified care. Together, we can make every moment meaningful for patients and families. Contact us today to learn how we can help you provide care and support for your patients who can benefit from hospice care.
Sources:
- American Heart Association, 2025.
- Palliative Care in Congestive Heart Failure- Sarah J. Goodlin Journal of the American College of Cardiology. Volume 54, Issue 5, July 2009. DOI: 10.1016/j.jacc.2009.02.078
- Journal of the American College of Cardiology (Palliative Care Heart Failure – PAL-HF Study, 2024)
- Medicare Hospice Benefit Guidelines, 2024
- Cross SH, Kamal AH, Taylor DH Jr, Warraich HJ. Hospice Use Among Patients with Heart Failure. Card Fail Rev. 2019 May 24;5(2):93-98. doi: 10.15420/cfr.2019.2.2. PMID: 31179019; PMCID: PMC6545999.
